When did the HMPV virus outbreak start?
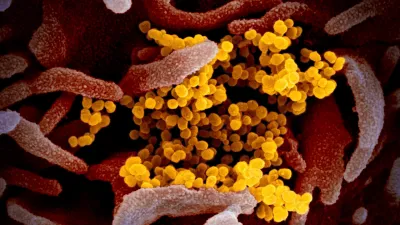
Five years after the onset of the COVID-19 pandemic, China is witnessing a surge in cases of Human Metapneumovirus (HMPV), predominantly affecting children under 14 years of age. The outbreak, which has raised concerns internationally, has been reported mostly in the northern provinces of China. Despite these developments, the Union Health Ministry of India has clarified that the situation in India remains stable, with no unusual spike in winter respiratory diseases.
When was the virus first discovered by medics?
HMPV, discovered in 2001 and part of the Pneumoviridae family, is known to cause upper and lower respiratory illnesses. Symptoms such as cough, fever, nasal congestion, and shortness of breath are common, with severe cases potentially progressing to bronchitis or pneumonia. According to Reuters, the outbreak in China has primarily impacted children, with cases peaking in colder regions.
Internationally, HMPV outbreaks have previously been recorded in the U.S., Canada, and Europe between 2011 and 2012. The virus is spread through respiratory droplets from coughing or sneezing, close personal contact, or touching contaminated surfaces before touching one’s mouth, nose, or eyes.
Is HMPV already in India?
The India National Centre for Disease Control is keeping a close watch on the global situation. They are monitoring respiratory and seasonal influenza trends within the country. Director-General of Health Services Atul Goel assured that no HMPV cases have been reported in India so far.
“HMPV is similar to other respiratory viruses that cause flu-like symptoms, primarily affecting children and the elderly,” Dr. Goel explained. “There is no need for alarm. Our healthcare infrastructure is well-prepared to handle routine respiratory illnesses during the winter season. Special medicines or antiviral drugs are not required since no targeted treatment for HMPV exists at present,” he added.
Global and Clinical Perspective
The U.S. Centers for Disease Control and Prevention (CDC) highlights that HMPV can infect people of all ages, with young children, older adults, and immunocompromised individuals being particularly vulnerable. The virus’s incubation period ranges from three to six days, and the illness duration depends on the severity, resembling other respiratory infections.
In the U.S., HMPV typically circulates during the winter and spring seasons, indicating its seasonal nature. The broader application of molecular diagnostic testing has heightened awareness of the virus’s role in causing respiratory illnesses.
Also read about HIV Breakthrough
Precautions and Public Awareness about the new outbreak
Experts emphasize preventive measures such as regular handwashing, avoiding close contact with infected individuals, and maintaining hygiene to curb the spread of respiratory viruses like HMPV. While the outbreak in China warrants monitoring, Indian health authorities remain vigilant, reassuring the public that the current situation is under control.
Health officials stress the importance of maintaining robust surveillance to prevent any unforeseen outbreaks. The Union Health Ministry continues to collaborate with international health agencies to stay informed about the evolving situation of the HMPV outbreak.
Comparison Between the new outbreak and COVID-19
Below is a detailed comparison of the similarities and differences between Human Metapneumovirus (HMPV) and COVID-19, organized into tables for clarity.
Similarities Between HMPV and COVID-19
| Category | HMPV | COVID-19 |
|---|---|---|
| Transmission | Spread through respiratory droplets and contaminated surfaces. | Spread through respiratory droplets, surfaces, and aerosols. |
| Symptoms | Fever, cough, nasal congestion, shortness of breath. | Fever, cough, nasal congestion, shortness of breath. |
| Affected Groups | Children, elderly, and immunocompromised individuals. | All age groups, especially elderly and those with comorbidities. |
| Complications | Bronchitis, pneumonia in severe cases. | Pneumonia, Acute Respiratory Distress Syndrome (ARDS). |
| Seasonality | Peaks during winter and spring. | Year-round spread with surges depending on variants. |
| Prevention | Hand hygiene, respiratory etiquette, and avoiding close contact. | Similar measures plus vaccination and mask-wearing. |
Differences Between HMPV and COVID-19
| Category | HMPV | COVID-19 |
|---|---|---|
| Causative Agent | Human Metapneumovirus from the Pneumoviridae family. | SARS-CoV-2, a coronavirus. |
| Discovery | Identified in 2001. | Identified in late 2019. |
| Incubation Period | 3-6 days. | 2-14 days, with most cases showing symptoms within 4-5 days. |
| Mode of Spread | Primarily respiratory droplets and contact with contaminated surfaces. | Also spreads via aerosols, allowing longer-distance transmission. |
| Testing Methods | Diagnosed using molecular tests or viral cultures. | PCR, rapid antigen tests, and genomic sequencing. |
| Severity | Generally mild; severe in young children and elderly. | Can cause mild to severe symptoms, including death. |
| Treatment | Supportive care; no specific antiviral drugs available. | Antiviral drugs (e.g., Remdesivir), monoclonal antibodies, and supportive care. |
| Vaccine Availability | No vaccines currently available. | Multiple vaccines developed globally. |
| Global Impact | Localized outbreaks; less widespread. | Pandemic-level impact across all continents. |
Preventive Measures (For Both HMPV and COVID-19)
| Preventive Action | Explanation |
|---|---|
| Hand Hygiene | Wash hands frequently with soap and water or use hand sanitizers. |
| Respiratory Etiquette | Cover mouth and nose when coughing or sneezing, dispose of tissues properly. |
| Avoiding Crowded Places | Reduces the risk of transmission in high-density areas. |
| Surface Disinfection | Regular cleaning of frequently touched objects and surfaces. |
| Health Monitoring | Seek medical attention if respiratory symptoms worsen. |
Summary
While HMPV and COVID-19 share some similarities in their symptoms and transmission routes, they differ significantly in their severity, global impact, and availability of preventive tools like vaccines. Understanding these distinctions helps in tailoring public health responses to each virus effectively.




